Deliberate Self-harm
Any child or young person who self-harms or expresses thoughts about this or about suicide has to be taken seriously and appropriate help and intervention offered at that point.
1. Introduction
1.1 Over the past three decades Childline has seen a major shift from children being bullied, neglected or abused to hearing from young people who are just ‘deeply unhappy'. Mental health issues dominate the main concerns which young people contact Childline about, with 109,136 counselling sessions relating to emotional health and well-being. Childline Annual Review 2018/19
2. Definition of self-harm
2.1 In this document the words “self-harm” are used to cover acts of self-poisoning or self-injury which may or may not be deliberate or include a wish to die. Most young people who self-harm do not intend to risk their lives and most self-harming behaviour is unlikely to lead to death. However, it is also important to note that some young people do die. The term ‘young people’ is used to include ‘children and young people’ up to the age of 18 years.
3. What is self-harm?
3.1 Self-harm describes a wide range of damaging things that young people do to themselves in an often deliberate and usually hidden way. The intention may not be to take one’s own life, however it must be noted that self-harm can be a common precursor to suicide and also that young people who self-harm may kill themselves by accident.
3.2 Attempted suicide is self-harm with the intent to take life, resulting in non-fatal injury. Suicide is self-harm resulting in death. Other self-harming actions might include;
- Cutting or scratching with knives, razor blades or other sharp implements
- Deliberately taking overdoses of drugs, or swallowing other substances
- Burning oneself with, for example, flames, heated metal, wax or chemicals
- Hitting or banging one’s arms, legs or head on walls, or with fists or objects
- Putting objects under the skin or elsewhere in the body e.g. needles
- Taking risks with the intention of hurting oneself which may also increase the risk of exploitation
- Self-strangulation
4. Why do young people self-harm?
4.1 People self-harm for many reasons and everybody’s experience is different.
- Can be a method of coping or validating emotional pain or psychological trauma like abuse
- Can be a way of surviving overwhelming feelings of helplessness and powerlessness; feelings are numbed or released by self-harming in order to survive a deeper despair.
- Is not necessarily a precursor to suicide (but may be). Self-harm is often a means of staying alive, rather than trying to take one’s life.
- Takes place across all ages, genders and backgrounds
- Is often hidden very carefully and many people do not seek medical care
5. Self-harm & Stigma
5.1 Self-harm is often stigmatised because people find it difficult to understand and empathise with. While many mental health problems have an invisible label, people who self-harm often have scars or other visible signs that make them noticeable in public. Many people hide their scars obsessively to prevent the negative consequences of them being seen.
5.2 The effect of public disgust and judgement that can lead to a further reduction of confidence and self-esteem and promotes the cycle that leads to self-harm in the first place; preventing some young people from speaking out.
6. Assessing the risk of suicide and self-harm
6.1 Self-harm and attempted suicide are complex issues and despite all interventions, policies and guidance based on the current evidence base will not prevent all suicide and self-harm. The management of young people who self-harm requires a multi-agency response. Suicidal thoughts and intention can be inconsistent and fluctuate depending on life events and other circumstances. A young person can feel so overwhelmed and helpless that the future appears hopeless; they may think suicide is the only solution to their situation. Depression is a major risk factor for suicide although not everyone who attempts suicide is depressed. Self-harm can be a coping mechanism for dealing with overwhelming emotions.
| CONSIDER THE POSSIBILITY OF EXPLOITATION IN ALL CASES |
The following identifies some commonly accepted risk factors for suicidal thinking and self-harm in young people;
- Exploitation – either criminal or sexual
- Previous suicide attempt or a family member / close friend / partner has committed suicide
- Discrimination
- Mood disorder
- Experience of physical, sexual or emotional trauma
- Family difficulties and/or not living with their original family
- Stressful life events e.g. significant loss / bereavement / relationship break-up /pregnancy
- Drug, alcohol and solvent usage
- Issues affecting young people who are gay, lesbian, bisexual and transgender
- Academic failure
- Problems involving violence
- Someone who stops ‘self-harming’ might still have a deep rooted problem they can’t cope with
- Parents with a mental disorder, harmful drug use or problems involving violence
- Chronic illness and disability
- Bullying
- Internet use / social media / cyber bullying
7. Defining if it is self-harm or attempted suicide?
7.1 Uncertainty in this area is common and staff should adopt the following approach; where the young person is expressing suicidal thoughts and /or their mood is negative they should be treated as being at risk of suicide. Any communication of distress should be taking seriously.
7.2 Listening to young people and trying to understand how life seems for the distressed person is the most important way of helping. Evidence shows that some teenagers may make a repeat suicide attempt when no one has really listened or where no help has been offered.
7.3 Being heard and understood is clearly stated by young people as being the most important and effective way of helping them. When caring for people who repeatedly self-harm, professionals should be aware that the individual's reasons for self-harming may be different on each occasion and therefore each episode needs to be treated in its own right.
7.4 Staff should provide a non- judgemental and confidential response; don’t be influenced by personal emotions or by your own prejudice or bias. Help the young person access the most appropriate service to meet their individual needs at the right time. Professionals should involve people who self-harm in all discussions and decision making about their treatment and subsequent care.
7.5 When assessing people who self-harm, professionals should ask young people to explain their feelings and understanding of their own self-harm in their own words and provide full information about the different treatment options available. People who have self-harmed should be offered treatment for the physical consequences of self-harm, regardless of their willingness to accept psychosocial assessment or psychiatric treatment.
7.6 Young people who self-harm should be allowed, if they wish, to be accompanied by a family member, friend or advocate during assessment and treatment. However, the initial psychosocial assessment should take place with the service user alone to maintain confidentiality and to allow discussion about issues that may relate to the relationship between the service user and carers.
8. Information sharing and consent
8.1 Informed consent to share information should be sought if the young person is competent unless:
- The situation is urgent and there is not time to seek consent
- Seeking consent may cause harm to someone or prejudice the prevention or detection of serious crime
8.2 All people over the age of 16 are presumed to have capacity to give or withhold their consent to sharing of confidential information, unless there is evidence to the contrary under the Mental Capacity Act 2005.
8.3 If consent to information sharing is refused (or cannot be obtained) then information should still be shared in the following circumstances:
- There is a reasonable belief that not sharing information may result in serious harm to the young person or to someone else
- Where not sharing information may prevent the detection of a serious crime
- There is significant harm to a child/ young person
8.4 Parents should be kept informed and involved in decisions about sharing information even if the child is competent or over 16. However, a competent young person’s wishes should be respected if they choose to limit the information given to his parents; unless conditions for sharing without consent apply. When a child or young person is not deemed competent a person with parental responsibly should give consent unless the circumstances for sharing without consent apply.
9. Equality & diversity and self-harm
9.1 Cultural sensitivity and awareness of identity is important when working with young people who self-harm from different black and minority ethnic (BME) communities. Communities or groups that experience issues relating to a loss of cultural identity, racism and discrimination are more likely to experience mental distress than those who do not. Practitioners need to be sensitively aware of this diversity. General characteristics of cultural groups that can inform a culturally appropriate service delivery may include:
- language and religion
- individual or collective orientation of the family’s cultural group
9.2 In relation to language, interpreters and translators are essential to help people access services.
10. Staff training and supervision
10.1 All professionals who have contact, in the emergency situation, with people who have self-harmed should be adequately trained to assess mental capacity and to make decisions about when treatment and care can be given without consent. Clinical and non-clinical staff who have contact with people who self-harm in any setting should be provided with appropriate training to equip them to understand and care for people who have self-harmed. People who self-harm should be involved in the planning and delivery of training for staff.
10.2 Providing treatment and care for people who have self-harmed is emotionally demanding and requires a high level of communication skills and support. All staff undertaking this work should have regular clinical supervision in which the emotional impact upon staff members can be discussed and understood.
11. Staff working with under-18s
11.1 Staff who have emergency contact with children and young people who have self-harmed should be adequately trained to assess mental capacity in children of different ages and to understand how issues of mental capacity and consent apply to this group. They should also have access at all times to specialist advice about these issues.
12. Your responsibility
12.1 The recommendations in this guidance represent the view of NICE; when exercising their judgement, professionals are expected to take these recommendations fully into account, alongside the individual needs, preferences and values of their patients. The application of the recommendations in the flowchart is at the discretion of professionals and their individual patients and do not override the responsibility of professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
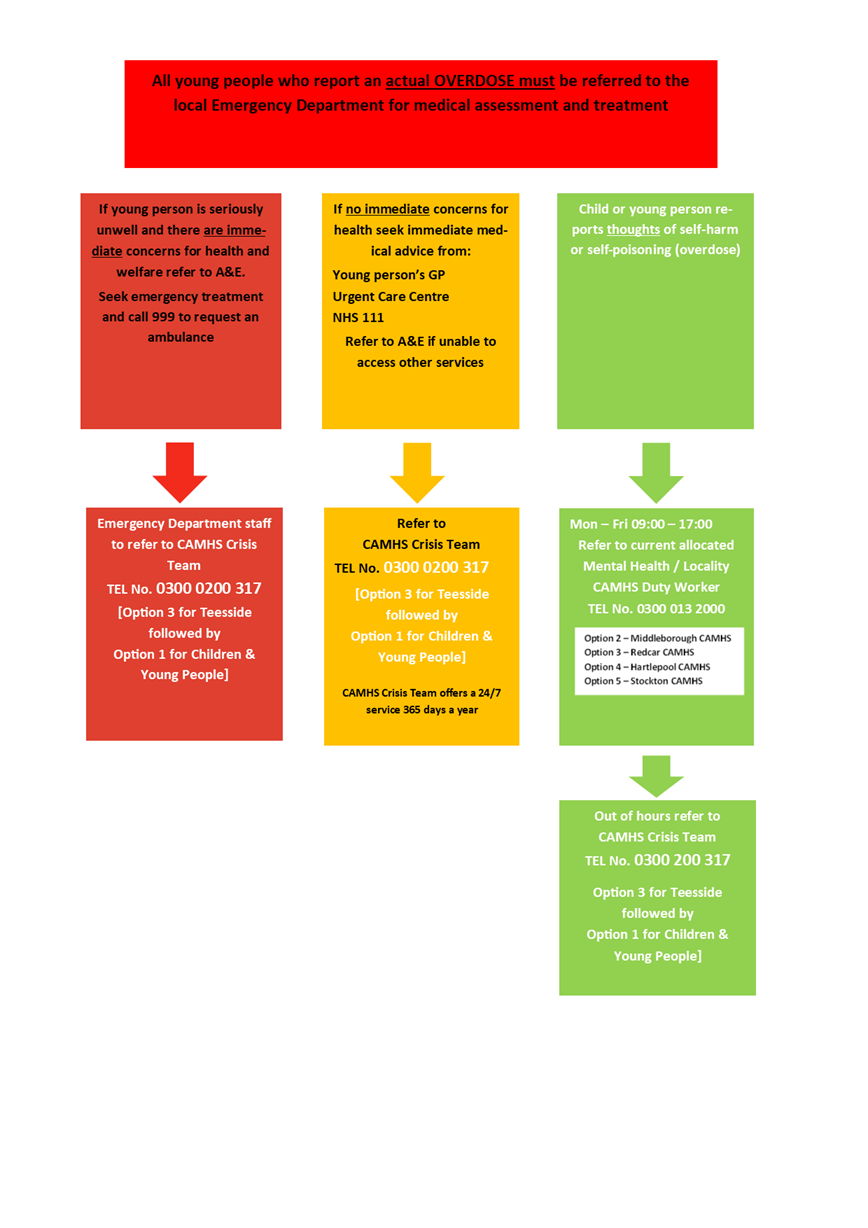
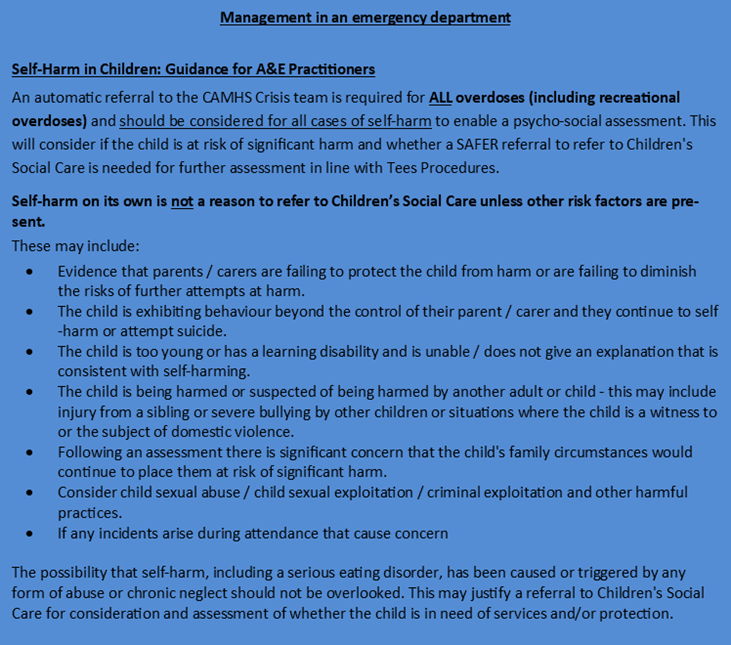
13. Multi-agency pathway for self-harm in children
Useful Tools/Pathways, Contacts and Websites:
- Child line for young people in trouble or danger. Freephone, 24 hours, 0800 1111
- Eating Disorders Association – now called BEAT – Information and support
- MIND info line Information on mental distress and treatment including self-harm. Monday – Friday, 9.15am – 5.15pm - 08457 660 163
- National Self harm Network – Provides a selection of literature and campaigns for people who self-harm. PO Box 16190, London, NW1 3WW
- Sane line – Info and advice on mental health issues including self harm and eating disorders
- Self-harm and Related Issues
- The Samaritans – 08457 909 090 (24 hours)
- Young Minds – for young people's mental health
- For more information on self-harm, see the Mental Health Foundation's Truth Hurts report (2006)