Bruising on Non Mobile Babies Procedure
Bruising in non-mobile children is rare and there is therefore a significant risk that bruising may indicate or neglectful care. Unfortunately, nationally and locally bruising is not always responded to appropriately by Practitioners. As a result a significant number of abusive events have been missed resulting in children being place at risk, serious untoward incidents and serious case reviews. This procedure sets out to address this by requiring all professionals to refer bruising in non-mobile children for assessment by a Children's Social Care and a Consultant Paediatrician.
1. Introduction
1.1 This procedure highlights that babies who are not yet mobile, but are observed to have bruising, should be of particular concern in terms of child protection.
1.2 Caution is advised, even in children who are mobile, and where there are concerns or doubts, a Consultant Paediatrician should be asked to evaluate the evidence. Emphasis is made on looking at any injury within the context of the child's social history and the parental/carer explanation.
1.3 Any bruising, or a mark that might be bruising, in a child of any age who is not independently mobile, that is brought to the attention of any professional (including GPs) should be taken as a matter for inquiry and concern and should result in an immediate Referral to Children’s Social Care and an urgent paediatric opinion sought.
1.4 'It should be acknowledged that on occasions it can be difficult to know if a skin lesion is suspicious or not e.g. Congenital Dermal Melanocytosis/Slate Grey Naevi (Mongolian Blue Spots), haemangioma. Where there is diagnostic doubt regarding the nature of a skin mark or lesion, a referral should be made to the child's GP. A decision should then be made about whether to proceed automatically to Children’s Social Care referral or obtain a Paediatrician Medical Review (same day) of the lesion first being observed.
2. Definitions
2.1 Non-mobile Baby: A baby who is not yet rolling, crawling, bottom shuffling, pulling to stand, cruising or walking independently. The younger the child the greater the risk the bruising is non-accidental and the greater potential risk of future harm. Please be aware that non-mobile babies are unable to roll independently.
2.2 Not Independently Mobile: Children with a disability – older children who are not independently mobile by reason of a disability should be considered. Children with disabilities may have a higher incidence of abuse whether or not they are mobile. This procedure does not apply to children with a disability who are independently mobile in a wheelchair and who can give a consistent plausible explanation for accidental bruising.
3. Older Children
3.1 Some older children have not achieved independent mobility and therefore the assessment should take into account if there is a delay in development; if there is, they should be treated as not independently mobile.
4. Physical Injuries
4.1 The evidence base for other injuries to non-mobile babies, e.g. scratches, other marks, is less clear. If a professional notices any injury to a non-mobile baby, an explanation should be sought. If a practitioner has any concerns about any mark, caution should be exercised and discussion should be had with Children’s Services and/or paediatric services. Birth injuries or injuries caused by medical interventions such as cannula sites should always be documented in the child’s medical records Please see pathway.
5. Injuries to non-mobile infants
5.1 Any injuries are unusual in this age group, unless accompanied by a full consistent explanation. Even small injuries may be significant, and they may be a sign that another hidden injury is already present.
5.2 Such injuries include:
- Torn frenulum (small area of skin between the inside of the upper and lower lip and gum);
- Bleeding from ears nose or throat or history of these;
- Lacerations, abrasions or scars;
- Burns and scalds;
- Pain, tenderness or failing to use an arm or leg which may indicate pain and an underlying fracture;
- Small bleeds into the whites of the eyes or other eye injuries
5.3 These infants are most at risk of serious deliberate harm and as such require careful consideration.
5.4 Any evidence of physical injury in an immobile infant, warrants a referral to Children’s Social Care and a ‘on call’ Paediatric consultant same day assessment on paediatric day unit.
REMEMBER: An older infant with any of the above findings would also warrant CAREFUL consideration.
5.5 A small percentage of bruising in non-independently mobile children will have an innocent explanation. Occasionally spontaneous bruising may occur as a result of a medical condition. Nevertheless because of the difficulty in excluding non-accidental injury in immobile infants practitioners should seek advice from a consultant paediatrician via Children’s Social Care in all cases. Child Protection issues should not delay the referral of a seriously ill child to acute paediatric services. An immobile child with bruising needs to be seen the same day by a Paediatrician. If a child is in need of urgent medical care they should not delay sending them to hospital and the practitioner should inform social care so they can commence child protection discussions e.g. Strategy Discussions and if required Section 47 Enquiries.
5.6 It is the responsibility of Children’s Social Care in conjunction with the local acute or community paediatric department to decide whether the circumstances of the case and the explanation for the injury are consistent with an innocent cause or not. Children should NOT be referred to GP's for a decision as to whether any ‘bruising’ is accidental or otherwise.
6. Birthmarks
6.1 It is not always easy to identify with certainty a skin mark as a bruise in young babies. Less clear cut lesions such as Congenital Dermal Melanocytosis/Slate Grey Naevi (Mongolian Blue Spots) or birthmarks should be promptly discussed with the child’s Health Visitor or GP.
7. Referral
7.1 It is the responsibility of the first professional to learn of or observe the bruising to make the referral. Wherever possible, the decision to refer should be undertaken jointly with another professional or senior colleague. However this requirement should not prevent an individual professional of any status referring to Children's Social Care any child with bruising who in their judgement may be at risk of child abuse.
7.2 If a referral is not made, the reason must be documented in detail with the names of the professionals taking this decision.
7.3 All telephone referrals must be followed up in writing on a Safer Referral Form. The written referral must contain the same information that has been shared verbally. Children's Social Care will co-ordinate multi-professional information sharing and assessment.
7.4 A bruise/injury must always be assessed in the context of medical and social history, developmental stage and explanation given. Assessments will be led by Children's Social Care and a lead medical professional (local acute or community Paediatrician) to determine whether bruising is consistent with the explanation provided or is indicative of non-accidental injury.
8. Involving Parents / Carers
8.1 As far as possible, parents or carers should be included in the decision-making process, unless to do so would jeopardise information gathering (e.g. information could be destroyed) or if it would pose a further risk to the child.
8.2 In particular staff and volunteers should explain at an early stage why, in cases of bruising in non independently mobile children, additional concern, questioning and examination are required.
8.3 If a parent or carer is uncooperative or refuses to take the child for further assessment, this should be reported immediately to Children's Social Care. If possible the child should be kept under supervision until steps can be taken to secure his or her safety.
9. Flowchart - Protocol for the assessment of bruising and other possible injuries in ‘Non-Mobile’ Children
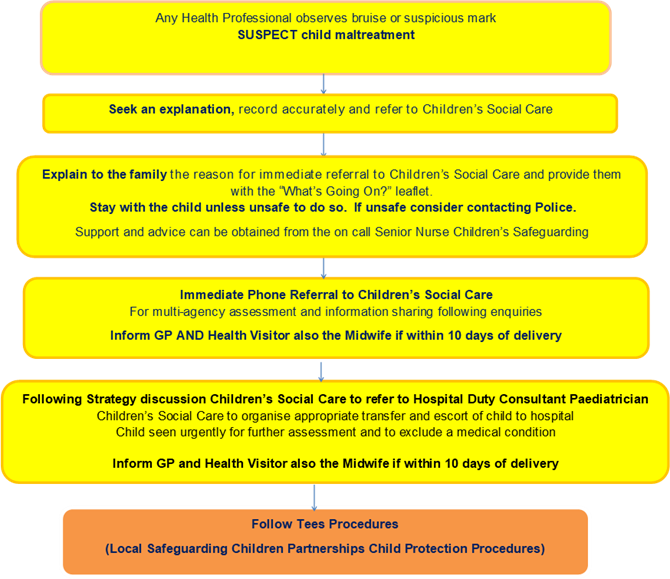
Hartlepool and Stockton-on-Tees Children's Hub: 01429 284284 / 01642 130080 / childrenshub@hartlepool.gov.uk
Middlesbrough MACH: 01642 726004 / MiddlesbroughMACH@middlesbrough.gov.uk
Redcar and Cleveland MACH: 01642 130700 / RedcarMACH@redcar-cleveland.gov.uk
Emergency Duty Team number for all 4 LA’s: 01642 524552
10. Useful Guidance Pathway Tools, Contacts and Websites:
- Pathway of care regarding suspected birth mark including Congenital Dermal Melanocytosis/Slate Grey Naevi (Mongolian Blue Spots)
- Bruising in Children Pathway
- What's Going On Leaflet - Bruising in infants who are not independently mobile: Information for parents and carers leaflet (NTHFT)
- NICE guidance When to Suspect Child Maltreatment.
- NSPCC – Core Information Bruising on Babies
- NSPCC 2011, All Babies Count: prevention and protection for vulnerable babies